In preparation for autologous blood stem cell transplant after 2024, I had my red blood stem cells harvested. The procedure was successful and that is the bottom line. That final tally was the result of very many debits and credits. Even though we had this planned months ago, when I was wheeled from the transplant clinic to the main hospital to be taken to radiology for the placement of a catheter, the main desk asked if I was a walk-in. It took them a couple of hours to find a file folder with papers that then were entered into a computer file. That was just one event.
I went to the Sarah Cannon Clinic at Methodist Hospital in San Antonio about 68 miles from home because the Sarah Cannon Clinic at St. David’s Hospital in Austin about 18 miles away will not harvest and store. At Methodist they were proud to tell me that they store stem cells for the other clinic. I do not know why that treatment was denied to me in Austin but it was. “We do not harvest and store. If we harvest, we use them.” So, we scheduled treatment down the road.
I met Methodist Hospital last year, after my initial diagnosis because the arithmetic of chance favors the second opinion. I have been happy to be treated here in Kyle because the office of Texas Oncology here is a short walk through a city park. It is very convenient. Even so, the second opinion has been helpful. (See “The Monty Hall Problem” on Wikipedia and elsewhere.) It validated the treatment regimens and provided additional insights. So, I have been back half a dozen times for lab tests and consultations.
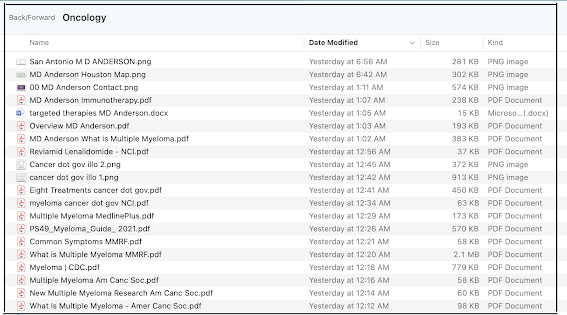
All along, I have taken as much charge of my treatment as I have bandwidth for. I bought textbooks and a microscope just for orientation because I never paid much attention to life sciences. I got a book from the UT library on oncology nursing just to read twenty pages on myeloma and Revlamid® (lenalidomide). You really have to ask the right questions to get any answer and many doctors control the flow of information according to their own standards. My primary oncologist assured me that this will not require chemotherapy and we will do it with monoclonal antibodies. He sounded like Dr. McCoy. Well, it is chemotherapy; I just don’t lose my hair (yet). And right now the FDA approves monoclonal antibodies only when two other courses have failed. So, OK, I got over that last year.
This time, the sugar coating was on the collection catheter, a Quinton line. I should have looked it up. “Oh, we’re just going to put a tube in your neck to collect blood...” In my neck, indeed, it went into my jugular and down to my superior vena cava. That much was fine, after all. It took two imaging systems (CT and fluoroscope) and an MD to place it. (I enjoyed listening to him cluck as he drove the twisty turny lane. I knew that he could do it.) “So,” I asked, “they can just take this out at the clinic?” Oh, yes, I was assured, after they remove it, they just hold the place shut for five minutes. Well, it was ten minutes and 30 minutes no talking lying flat to make sure that it is not bleeding out and I have dressings to wear for 72 hours and I cannot lift more than five pounds. All of which is going to impact my first day of work on a new job Monday. Who knew?
All in all, there are worse outcomes. I am reminded of a comedian I saw on a late night show who told of a woman seated next to him on an airliner, on a telephone, telling her friend about having “the worst day of my life” while reclining in a cushioned couch at 38,000 feet, traveling 80% the speed of sound.
My daughter reminded me of Adm. William H. McRaven’s parable of the sugar cookie. (See "Make Your Bed.") Other people tell it differently but for McRaven the point was that being chosen to be hosed down and rolled in the sand and spending the rest of the day covered like a sugar cookie has nothing to do with any choice you made. You could not have seen it coming and you could not have avoided it. It just happened to you. Sometimes, life is like that. So, get over it.
And on the assets side, every one of the nurses and assistants who were my direct caregivers were capable, informative, engaging, and supportive. I enjoyed talking to all of them. Not only do I like talking about myself but I am pretty good at interviewing and I ask a lot of questions. One of my radiologists was injured in college sports and went back for a second degree. One of the consulting oncologists was a Navy doctor. I had at least a dozen great interactions over the past three months.
I have been told that there are many ways to view multiple myeloma. “This is not like breast cancer. You don’t have a lot of options here. This thing is just going to run its course.” On the other hand: “Think of it like diabetes: just something you have to manage for the rest of your life.” When I was diagnosed my initial research warned me that almost half of patients have an expected end-of-life of less than one year. It is also true that the other half, 52% or more, live ten years and more. The statistical tail on the right is getting longer.
PREVIOUSLY ON NECESSARY FACTS
Disruptive Diagnostics and the Business of Science